Leucovorin, a prescription drug traditionally used alongside chemotherapy, has moved from a niche medical role into a highly charged public debate over its potential use in children with autism spectrum disorder. The renewed attention has been driven by regulatory signals, parental advocacy, and small clinical studies, yet the scientific foundation remains incomplete. As prescriptions rise and supply tightens, clinicians and policymakers are being forced to confront how evidence, demand, and regulation intersect when hope outpaces proof.
Regulatory signals and the rise of off-label use
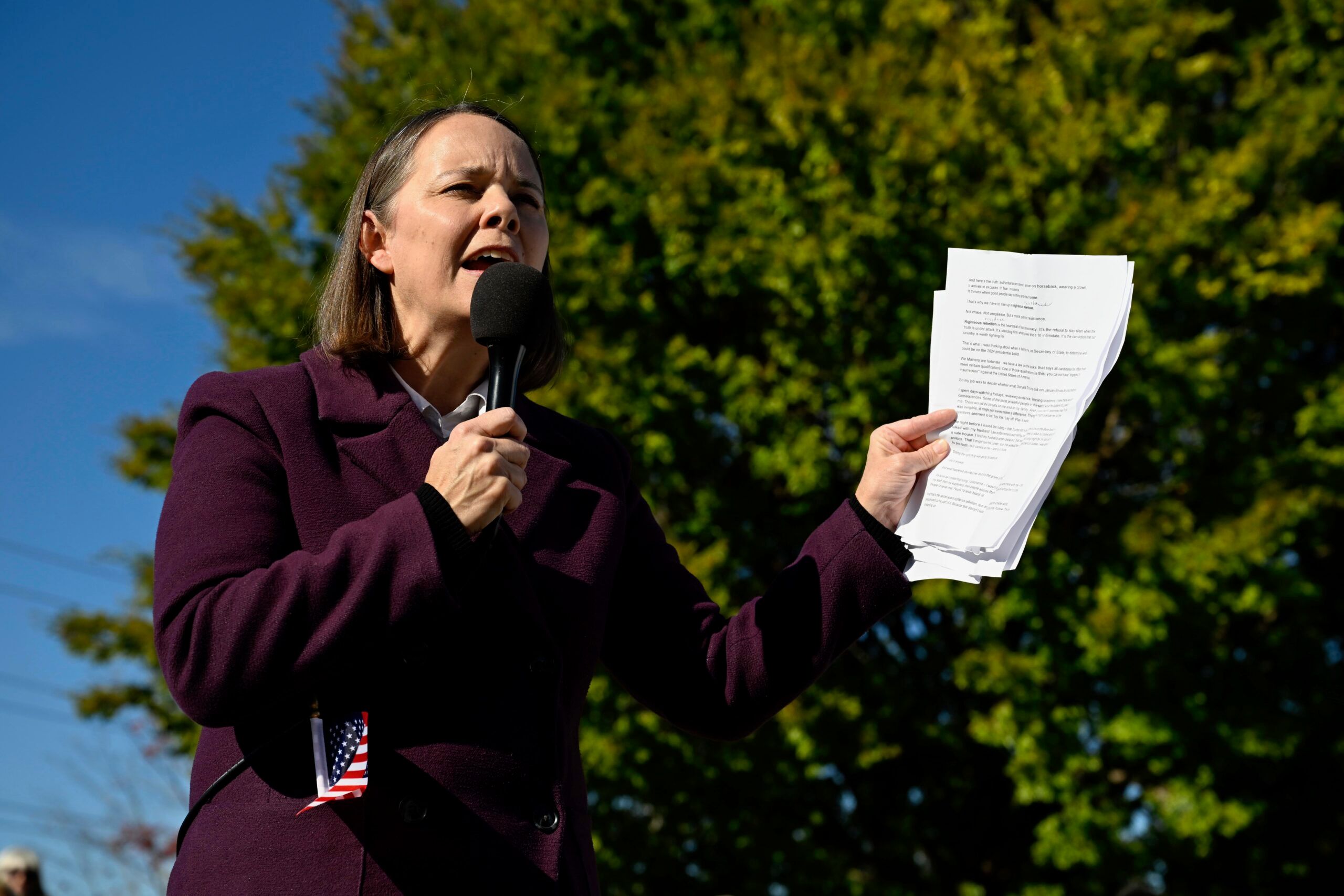
Momentum around leucovorin intensified after senior federal officials publicly suggested that the drug could eventually be made more accessible for children with autism, even though no formal label change has been approved by the Food and Drug Administration. In the absence of regulatory authorization, physicians have relied on off-label prescribing, a legal but controversial practice that shifts responsibility from regulators to individual clinicians and families.
This surge in interest has had tangible economic effects. Supply constraints have emerged as demand increased, pushing pharmacies and health systems to rely on imported alternatives. Temporary measures to stabilize access have highlighted how quickly a single regulatory comment can ripple through markets, particularly when annual treatment costs can reach several thousand dollars per patient, often exceeding $3,000 to $5,000 per year depending on dosage and insurance coverage.
The science behind folate pathways and autism
The biological rationale for leucovorin centers on folate metabolism and a condition known as cerebral folate deficiency. Folate plays a critical role in early brain development, and disruptions in how folate reaches the brain have been linked to neurological symptoms. Research published in leading medical journals, including studies indexed by the National Institutes of Health, has explored whether immune-mediated mechanisms could block folate transport, potentially contributing to developmental disorders.
Small trials have reported improvements in specific symptoms, such as language function, in subsets of children receiving leucovorin. However, these studies were limited in size and duration, and they did not establish consistent diagnostic criteria for identifying which children might benefit. Larger reviews of autism research, including those summarized by the World Health Organization, emphasize that autism is a heterogeneous condition, making it unlikely that a single pharmacological intervention would address core symptoms across the spectrum.
Historical caution and unresolved questions
The enthusiasm surrounding leucovorin echoes earlier cycles in autism treatment, where biologically plausible therapies gained popularity before rigorous trials failed to confirm meaningful benefits. Medical historians note that similar excitement once surrounded other supplements and hormonal therapies, many of which ultimately showed no advantage over placebo when tested at scale.
Professional organizations such as the American Academy of Pediatrics continue to advise caution, stressing that evidence remains insufficient to support routine use of leucovorin for autism. Beyond clinical uncertainty, ethical and economic considerations loom large. Families may invest thousands of dollars annually in therapies that offer unclear returns, while public confidence in regulatory oversight risks erosion if expectations are not carefully managed.
As new trials are planned and advocacy grows louder, leucovorin sits at the intersection of scientific inquiry and public pressure. Whether it will ultimately secure a defined role in autism care depends not on momentum, but on the slow, exacting work of controlled research and transparent regulation.