Scientists have taken a major step toward understanding one of the most elusive stages of human development: how an embryo implants in the uterus. By recreating highly controlled, womb-like environments in laboratory settings, researchers are now able to observe implantation in real time. This was previously impossible due to the inaccessibility of the early human womb. This breakthrough is reshaping scientific knowledge about early pregnancy. It could redefine how infertility and miscarriage are studied and treated.
The experimental systems, often described as “womb-on-a-chip” platforms, simulate key biological conditions found in the uterine lining. These models allow embryos and embryo-like structures to interact with human endometrial tissue under tightly regulated conditions. Consequently, they reveal molecular signals and cellular behaviors that were once hidden. Research institutions and biomedical innovators working in reproductive science have long highlighted implantation as a critical bottleneck in successful pregnancies. This issue is explored extensively by organizations such as https://www.nichd.nih.gov, which focuses on human development and reproductive health.
How artificial womb systems replicate early implantation
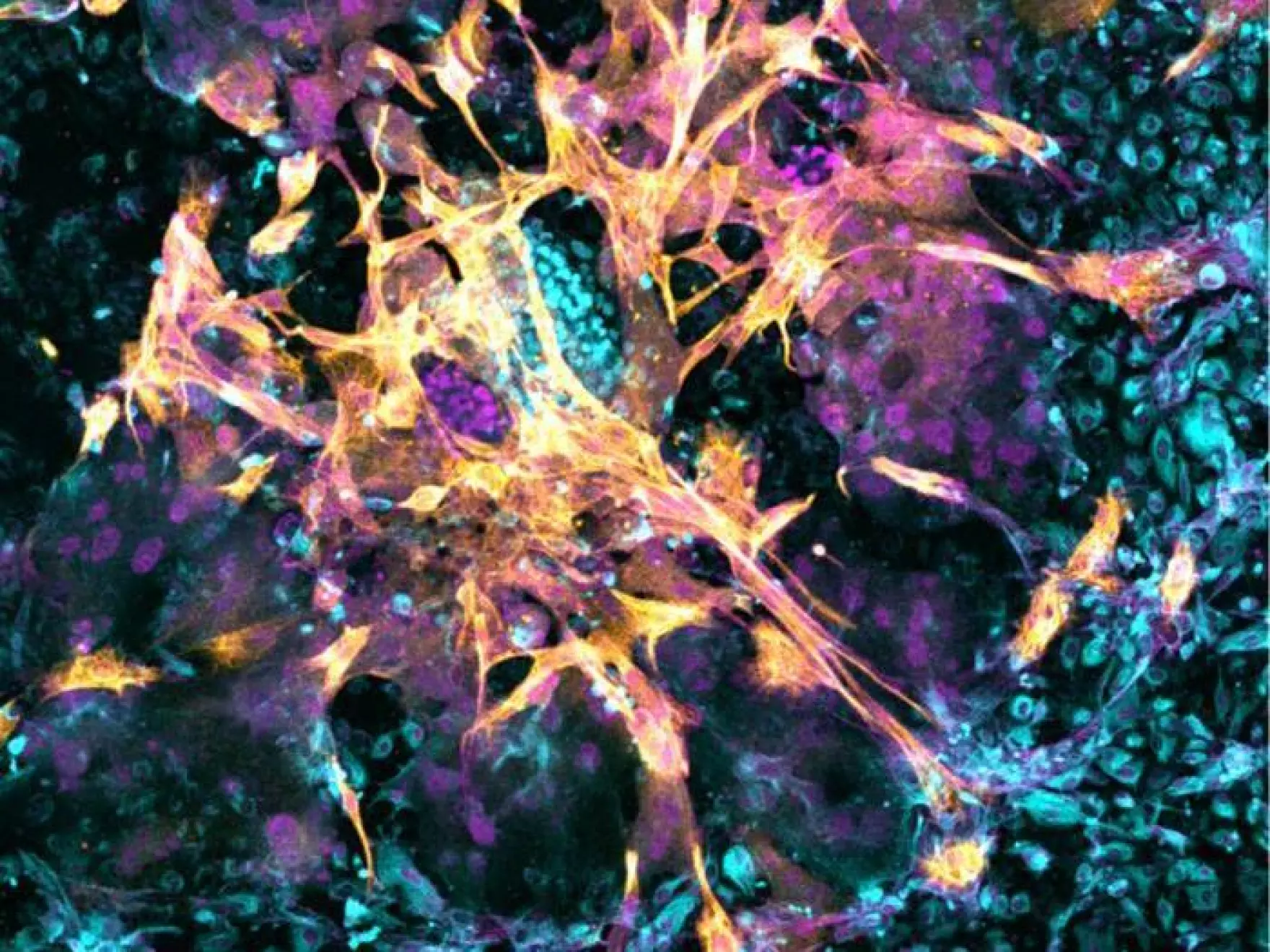
At the center of this scientific progress is the ability to recreate essential features of the uterine environment using microengineered devices. These systems incorporate human cells obtained during routine medical procedures and organize them into functional layers that mimic the structure of the uterine lining. When embryos or stem-cell-derived embryoids are introduced, scientists can track attachment, invasion and early differentiation processes at a cellular and molecular level.
This approach has allowed researchers to observe the full sequence of implantation events, from initial contact to deeper embedding into the simulated uterine tissue. Such insights are particularly valuable because implantation failure is believed to be a leading cause of early pregnancy loss. According to reproductive health research summarized by https://www.who.int, millions of pregnancies worldwide end in miscarriage each year. They often occur without a clear medical explanation.
In addition to observation, these artificial womb platforms enable large-scale testing. Scientists have screened more than 1,100 compounds to identify drugs that may improve implantation success or prevent early pregnancy failure. This kind of high-throughput testing would be impossible in traditional clinical settings. Ethical and biological constraints limit experimentation on early embryos.
New possibilities for infertility treatment and pregnancy health
The implications of this research extend well beyond basic science. By comparing artificial womb environments built from healthy uterine tissue with those derived from women who experienced miscarriages, researchers have been able to directly observe implantation failures as they occur. This comparative approach is generating new hypotheses about why some embryos fail to implant even when they appear genetically normal.
The findings could influence the future of fertility treatments, including in vitro fertilization, a global market estimated to be worth more than $25 billion annually. As fertility clinics continue to seek higher success rates, insights from artificial womb research may guide personalized treatment strategies. They can also optimize embryo selection and improve uterine preparation protocols. Broader trends in fertility innovation and reproductive biotechnology are tracked by platforms such as https://www.statista.com, which documents the rapid growth of assisted reproductive technologies worldwide.
Beyond fertility care, the research offers a window into fundamental human biology. Implantation triggers a cascade of developmental events that determine how tissues and organs form later in pregnancy. Understanding these early steps could eventually lead to preventative strategies for developmental disorders that originate in the earliest days of life.
Ethical concerns and the boundaries of embryo research
While the scientific potential is substantial, artificial womb research also raises complex ethical questions. One of the most sensitive issues is how far embryo development should be allowed to proceed outside the human body. Many countries adhere to a 14-day rule that limits embryo research beyond a specific developmental stage. This boundary continues to shape global bioethics discussions led by institutions such as https://www.hastingscenter.org.
There are also concerns about the long-term implications of ectogenesis, the theoretical ability to support embryo and fetal development entirely outside the human womb. Although researchers involved in current studies emphasize that such applications remain far from reality, some ethicists argue that incremental advances could eventually make extended external development technically feasible. This possibility has sparked debate about the moral status of embryos. There is concern over the risk of commodification and the governance structures needed to regulate emerging reproductive technologies.
At the same time, scientists working in the field stress that their primary goal is understanding early pregnancy, not replacing natural gestation. They point to parallel advances in neonatal care, where artificial womb-like systems are already being explored to support extremely premature infants. This is evidence that biomedical innovation often progresses faster than ethical consensus.
As artificial womb research continues to evolve, it sits at the intersection of scientific discovery, medical innovation and ethical reflection. By illuminating the earliest moments of human development, these technologies are expanding the boundaries of what can be known. At the same time, they also challenge society to define how such knowledge should be used.