The United Kingdom has become the first country to legally implement three-parent IVF to prevent the transmission of mitochondrial diseases. So far, eight children have been born using the technique, which involves combining the DNA of two parents with healthy mitochondria from a donor egg. This innovative method is designed to prevent the inheritance of mitochondrial conditions that can cause severe developmental issues, organ failure, and premature death.
Three-parent IVF is tightly regulated in the UK and currently available through specialized clinics under strict ethical guidelines. The treatment has been life-changing for families carrying mitochondrial mutations, offering a chance to have genetically related children without the burden of hereditary illness.
Learn how mitochondrial donation works
How Three-Parent IVF Works
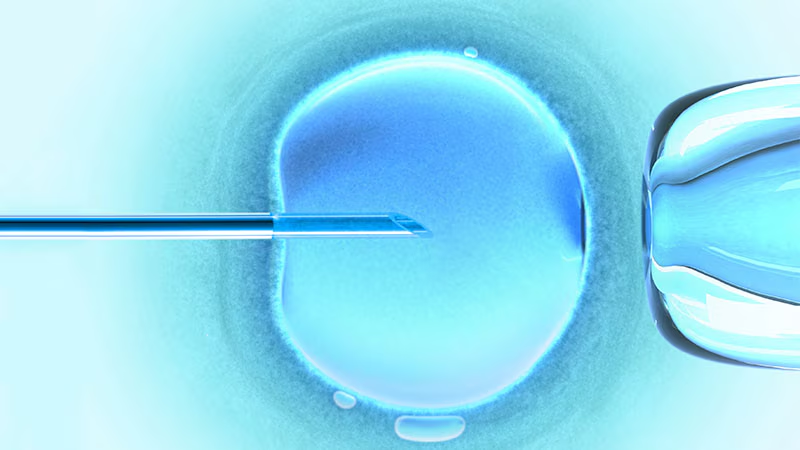
The process involves transferring the nuclear DNA from the parents’ embryo into a donor egg that contains healthy mitochondria but no nuclear DNA. This results in an embryo with more than 99.9% of its DNA from the biological parents and only a small portion—mitochondrial DNA—from the donor. The donor DNA plays no role in the child’s appearance or traits but is essential for cellular energy production.
Mitochondrial diseases are often fatal or severely disabling, and they affect approximately 1 in 5,000 people globally. By replacing damaged mitochondria, this approach drastically reduces the risk of transmission. The outcomes so far have been encouraging, with no reports of mitochondrial-related illness in the children born through this method.
For more on the science behind the treatment, visit the Science Media Centre.
Ethical Framework and Regulation in the UK
This groundbreaking therapy is legal in the UK under legislation passed in 2015. It is closely monitored by a regulatory authority that assesses each application on a case-by-case basis to ensure it meets ethical and medical standards. Clinics must demonstrate that no alternative treatments are available and that there is a high risk of serious mitochondrial disease being passed on.
A bioethics council has previously concluded that mitochondrial donation is ethically acceptable under proper safeguards. The focus remains on preventing disease rather than enhancing human traits, which helps distinguish it from more controversial genetic modifications.
You can learn more about ethical oversight and patient protections on the Nuffield Council on Bioethics website.
Looking Ahead: Broader Implications for Global Healthcare
The success of the UK’s mitochondrial donation program is likely to influence international reproductive policy. Other countries are already considering similar frameworks. While some remain cautious due to long-term safety unknowns, the UK’s experience may serve as a model for ethical implementation elsewhere.
As more data emerge from the ongoing monitoring of children born through this process, medical professionals anticipate further refinements in technique and expanded access. There is also growing interest in applying related methods to other hereditary conditions in the future.
For a deeper dive into clinical research, visit the University of Newcastle’s medical science division.